As we are approaching the cold and flu people will be flooding the pharmacy aisles to stock up on their arsenal of medications. A common dilemma they will encounter is multiple medications which have the same ingredients in them. From pills to liquids to suppositories, acetaminophen is an ingredient in over 600 medications. According to website Know Your Dose.Org "almost 50% of the unintentional overdose of acetaminophen are directly related to people failing to read and follow the label directions." Labels provide you with instructions as how it should be taken, the active and inactive ingredients and other important information.
Learn more about "Reading Your Label" for both over-the-counter as well as prescription medications. Until next time...NAMASTE.
Tuesday, October 27, 2015
Monday, October 26, 2015
Collaborating for better care
On March 23,
2010 President Obama signed into law the Patient Protection and Affordable Care
Act (PPACA), commonly called the Affordable Care Act and otherwise referred to
as Obamacare. PPACA was designed to be the financial, technological, and
clinical transformation of hospitals and primary physician practices. The goal
of PPACA was that healthcare would be more affordable and accessible for all
people as well as it would decrease the financial impact of healthcare on the
government. Theoretically it sounded good, however there is a major glitch in
the system which has prevented it from attaining an important component of the
overall goal, a decreased emergency room (ER) visits. According to a May, 2015 USA Today article,
three quarters of ER physicians report surge in ER visits since PPACA became
effective.
You may be
asking yourself, if more people have medical coverage under PPACA, why ER
visits would be on the rise. The answer, projected to be a problem before
PPACCA’s implementation, is the insufficient number of primary care physicians
to keep pace with the number of the newly insured. More and more, physicians
are opting out of primary care due to the level of reimbursement which does not
correlate fairly to the multi-services needed to provide optimal care. The lack
of a balanced patient/physician ratio means longer wait times for appointments
driving those in need of care, not necessarily emergency care, to the ER. The
other side of the story according to The American College of Emergency Medicine
press release is that 97% ER physician report treating Medicaid patients daily
who were unable to find a doctor willing to accept their insurance. Medicare is
not immune to this either as increasingly physicians are not accepting patients
with Medicare either. Even more frightening is a growing trend where physicians
are moving towards a direct pay/concierge practice (contract for service) where
the third party payer (insurances) are eliminated. My concern is are we beyond
the point of repair and if not what can be done to possibly correct it?
Admittedly,
countless attempts have been made by health care leaders and policy makers to
address eliminating fraud, checking errors, compelling following guidelines,
educating healthcare consumers, etc. with none having the desired impact. My concern is are we beyond the point of
repair and if not what can be done to possibly correct it?
Michael E.
Porter, a professor at Harvard Business School and Thomas H. Lee, MD, chief
medical officer at Press Ganey Associates in their article The
Strategy That Will Fix Healthcare have outlined a strategy which I believe
is worth considering. They emphasize to
create a successful strategy one must have concise goals. The main goal for
both healthcare providers and stakeholders should be improving value for
patients. Value should be defined by the outcomes that matter to healthcare
consumers in relation to the cost to achieve them. Raising value requires
improving the outcomes without increase in cost or lowering cost without
compromising the outcome. The strategy is a six step process:
·
Step
1. Organize into Integrated Practice Units (IPUs)
The
manner in which we deliver care needs to be transformed. Care should be
organize around the healthcare consumer’s needs and medical condition/s. IPUs
treat not only the condition but also all related conditions and complications
associated with it. An example would be the treatment of diabetes. Diabetics
also can have directly related eye and kidney problems. In addition to clinical
care there is also the need for educational and counseling services. This helps
to encourage patient engagement in their care as well as support to make
lifestyle changes. IPUs help eliminate fragmented care because services are
provided at one location and are coordinated by a team.
·
Step
2. The Cost and Outcomes for Each Patient Is Measured
The
outcomes and cost by condition is rarely tracked by providers or insurers. This
gives insight as to why reforms have failed to change the progression of usefulness
of the healthcare system. In those instances where measures are done, the focus
has mainly been in the area of mortality and safety. Using diabetes again,
providers gauge such things as lab values (A1C or LDL cholesterol) as outcome markers.
Yet for the diabetic what matters is maintaining vision, avoiding dialysis,
reducing their risk of a heart attack, stroke or the need for amputations.
These are the true markers to measure cost and outcome for diabetes.
·
3.
Bundled Payments for Care Cycles
The
two current payment systems, dominant payment or fee-for-service address, fail
to reward for improvement in the value of care. With the global payment system
(single payments for patient’s care) providers are rewarded for spending less.
Fee-for-service rewards providers for volume generated (how many of services
they provide) without consideration of value. Bundled approach reimbursement is
made to cover the full care cycle for a chronic condition over a specific
period of time (usually a year) or primary and preventive care for a defined
population (healthy children, adults
or seniors as an example). Bundled payments encourage both a team approach and
high valued care.
·
4. Integration of Delivery of Care System
In
2011, 69% of healthcare organizations were multi-site. Multi-site healthcare
organizations are generally stand-alone units that provide duplicated services.
By integrating systems there is a higher possibility of eliminating fragmented
and duplicated care, while optimizing the care delivered at the site. To
achieve such a system there are four things to consider – scope of services,
concentration of volume in fewer locations, matching the right service for
location, and integrating patient care across all locations.
·
5.
Expand Geographic Reach
The
delivery of care is generally localized to geographic areas. To provide
superior and specialized care to more individuals requires strategic expansion
of IPUs. Full service hospitals/practices focus on volume and not necessarily
improving value. One model for expansion is the creation of a hub-and-spoke
model. Main facilities (the center of the hub) handle more complex cases with
the satellite facilities (the spokes) handling the less complicated care. The other option is the clinical affiliation
model. The IPU partner with community providers or other local organization and
use their facilities. An example is the approach taken by MD Anderson. They
lease outpatient facilities on community hospital campuses utilizing the
hospital’s operating room and other inpatient and ancillary services as needed.
This is a win/win situation. The local affiliates benefit from the expertise of
the parent IPU and the IPU broadens their market share, regional reach and
referrals of complex cases.
·
6. Build an Enabling Information Technology
Platform
This
is perhaps the meat of the strategy…the ability to develop an interactive
supporting information system. History has seen failure in this area due to
complicated rather than integrated multidisciplinary care. The right IT-system
can help IPUs work together and tie all the parts of a well-structured delivery
systems together.
This strategy is being implemented
increasingly throughout the United States. Just recently a local facility in my
area became the “gold star” of cardiac care with the joint alliance between MedStar
Heart Institute and the Cleveland Clinic Heart and Vascular Institute.
According to Dr. Stuart F. Seides, the Heart & Vascular Institutes
Physicians Executive Director, “our whole is now greater than the sum of our
parts…with this alliance, the future of heart care in this region is
transformed”.
I envision the coming in of an era
where this is done for not just heart disease but for all aspects of care.
Please give me some feedback on
this one…until next time…NAMASTE.
Tuesday, October 20, 2015
Follow that Paper Trail
As a consumer in today’s healthcare system do you often feel
that the focus of care is volume instead of value? I do not know about you but
often I am left feeling like I am on a mass production assembly line. It
is not untypical to have a two hour wait in a doctor’s standing room only
waiting room; only to spend 15 minutes max with him/her. Few physicians have
the luxury of developing relationships with their patients where they really
get to know their full health story and often most people see more than one
provider. While strong patient-provider relationships lead to healthier
outcomes (Harvard
Business Review), few physicians are afforded this luxury. According to the American Health Insurance
Plan article “Rising Health Care Cost”
the system is not delivering service to correlate with the 2.7 trillion dollars
annually spent on health care. Approximately 20-30% is associated with care
which is wasteful, redundant or inefficient. So you may ask, what you can do to fix such a broken system. Now, do not get me wrong, this complex problem is
going to require a complex solution to repair but each one of us can play a
part in the process.
Time is a commodity in healthcare and in an emergency it can
be the difference between life and death. With having a system that is so
fragmented it can become almost impossible for one’s various providers to
remain abreast of all your health information. Laboratory, diagnostic scans and
x-rays results are only three examples of information that is beneficial for a
practitioner to have on your visit. Unfortunately the development of a
nationwide database which would enable all facilities to share such information,
which was proposed by Eric Schmidt CEO of Google in the summer of 2009, has not
come to fruition. So the responsibility of collecting this information is left
as a responsibility of you, the patient. To help ensure continuity in care throughout
your lifetime, no matter where you geographically may be, health consumers
should learn how to compile their own health information. This may seem
overwhelming but organizing
your records paperless can really simplify the process.
The concept of individuals collecting their personal health
information has been around for decades, referenced as early as 1956, but in
2000 the switch from paper to a paperless electronic application became trendy.
It is important to note that personal health records (PHRs) differ from
electronic health records (EHRs). EHRs are a software system used by health
care providers and health institutions which are a legal documentation of your
care. A PHR is a tool the health consumer can use to collect, track and share their
health information but is not considered a legal document. One could view a PHR
as a way to take an active role in monitoring your health story to better
collaborate your care.
There are a couple drawbacks in establishing your PHR and
perhaps the primary one is privacy. The manner in which one’s sensitive medical
information is stored and shared definitely raises concerns. Reputable data
systems follow the best privacy practices but any online based system cannot
claim to be 100% fail proof. The fact remains, even with such concerns, PHR’s
can save your life in an emergency situation. One such story is that of a woman
who had chronicled her medical information on her Facebook page (A women’s Facebook PHR
saved her life) and was used by emergency personnel when it was brought to
their attention by her son. There are externally devices, one example of this USB Medi-Chip, which might make someone
with privacy concerns more comfortable. This would be my preference. The second
biggest obstacle is time and commitment. It takes a considerable amount of time
to initially begin to document your information and it requires commitment to
keep the information updated and current. Updating would require any changes to
medications, all diagnostic test results and summaries of medical visits be
documented. This may seem like a lot of work but something like knowledge of a
medication allergy could be lifesaving if you ever become unable to convey such
information yourself.
Let there be no question of the importance of medical
information availability. Between 210,000 and 400,000 individuals died in the
United States in 2013 as a result of medical errors. Stephen Cobb, senior
security researcher at ESET North American, believes that access to a patient’s
medical record regardless of where they live, where they are being treated and
how many physicians they see would reduce accidental deaths due to these
errors.
Since the likelihood of such a national linked database is
slim due to the many privacy issues many feel it poses, the ball is left in
your court. Imagine 25 years from now someone asking you questions about your
medical history…trying to remember every detail will be like digging through a
stack of papers…difficult if not impossible to find. Believe more than likely
you will not be able to rely on memory alone. PHRs are the next best thing to
sliced cheese and everyone should invest the time to have one. Until next time…start
tracking your health information…NAMASTE.
Saturday, October 3, 2015
The Art of Brewing a Delighful Cup
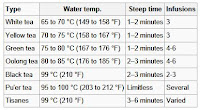
Perhaps you believe as I did that making a cup of tea involved just heating some water and pouring it over the leaves. I must confess before I got a hot water kettle, I heated water in the microwave. Yes, I did say the microwave. As I began reading up on the art of making a good cup of tea I found there are several factors involved in creating that perfect cup, with the water itself and the water temperature as key factors. Definitely heating the water in the microwave is a big DO NOT DO. Though loose leaf is preferred, quality tea can be found in loose and bagged teas.
Getting quality sleep at night has been a problem negatively impacting my health for many years. I have tried various different sleep aid teas, some working better than others to help me drift off into a sound sleep. I must say without a doubt,Vipova Tea has worked best me. If you have found one that achieves what you are looking for you may just want to stick with that one. Please, before you start comparing the cost of Vipova to other sleep aid teas, think of the evolution in the coffee industry. If I remember correctly, a cup of specialty coffee at a popular coffee establishment can cost you $5.00 a cup (depending on your pallet's desire) and they are not lacking for customers.
If you have not already noticed, I have put a banner for Vipova on the site. I will say if you are looking for a good quality tea that has health benefits, it may be worth trying it. I have a cup every night and my sleep quality is 90% better prior to my drinking it. I think I have to live with that 10% deficit which I attribute to aging. Some days I just can't get through the night without that bathroom pit stop :-).
You may also consider getting a good electric kettle so you get your water temperature as optimal as possible. After some research, trial and error, I have settled with the Cuisinart CPK-17 Perfect Temp. Of course a less expensive kettle can be found but the temperature settings, stainless steel design and the dripless pour spout are only a few attracting features it offers.
Both the teas and the kettle you choose should be considered as an investment to your commitment to better health...aren't you worth it. Hope to get some feedback on your Vipova or other tea experiences.
Until next time...happy brewing...NAMASTE.
Friday, October 2, 2015
You Play a Role In Preventing Medical Errors
One would want to believe within our advanced healthcare system, from the hospitals, clinics, pharmacies, and to your homes, errors are a rarity and do not occur as often as they do. According to the website Hospital Safety Score, hospital errors are the third leading cause of deaths in the US. I am not sure about you, but to me just taking into account hospitals alone, this is an alarming statistic. This screams to me a need for the healthcare consumer to be more proactive in regards to theirs and their loved ones safety. The Agency for Healthcare Research & Quality has created a Patient Tip Fact Sheet to help arm you with steps you can take to help ensure your safety in the healthcare battlefield.
I have always been a proponent of the power of QUESTIONS. ASK...ASK...AND ASK SOME MORE. When it comes to your health, the only silly question are the ones never asked. I also strongly advocate having a healthcare agent. This can be a trusted family member, friend, or a hired patient care advocate. This individual needs to have a thorough knowledge of your medical history. He/she could provide valuable information if you were every unable to do so. Your agent should be updated whenever any of your information changes (new provider, new or discontinued medication, etc.). If possible they should as often as possible accompany you to important medical visits, medical procedures and/or hospitalizations. Because privacy laws (HIPAA) limit the information a healthcare provider can share, be sure to sign the necessary legal documents which will give your agent access.
Today, take some time to consider how your safety may be at risk and what actions can you take to correct it. Let's get some dialogue going to share with others...I'll start with this question...you go to the pharmacy to pick up a medication...what should you do? One answer...verify the package given to you is really for you and the correct medication is inside. According to US New Health, one of the top pharmacy errors is the medication going to the wrong individual.
Remember it takes a village...until next time...stay aware...NAMASTE.
I have always been a proponent of the power of QUESTIONS. ASK...ASK...AND ASK SOME MORE. When it comes to your health, the only silly question are the ones never asked. I also strongly advocate having a healthcare agent. This can be a trusted family member, friend, or a hired patient care advocate. This individual needs to have a thorough knowledge of your medical history. He/she could provide valuable information if you were every unable to do so. Your agent should be updated whenever any of your information changes (new provider, new or discontinued medication, etc.). If possible they should as often as possible accompany you to important medical visits, medical procedures and/or hospitalizations. Because privacy laws (HIPAA) limit the information a healthcare provider can share, be sure to sign the necessary legal documents which will give your agent access.
Today, take some time to consider how your safety may be at risk and what actions can you take to correct it. Let's get some dialogue going to share with others...I'll start with this question...you go to the pharmacy to pick up a medication...what should you do? One answer...verify the package given to you is really for you and the correct medication is inside. According to US New Health, one of the top pharmacy errors is the medication going to the wrong individual.
Remember it takes a village...until next time...stay aware...NAMASTE.
Subscribe to:
Posts (Atom)